Release date: 2016-06-17

BACKGROUND: Chimeric antigen receptor T cells (CAR-T) are genetically engineered synthetic receptors that can be directed to cancer cell surface antigens to achieve cancer clearance. There are also many CARs that incorporate structures that enhance T cell activity and persistence. CAR-T cells have achieved great success in eradicating blood-based cancers, such as CD19-specific CAR-T therapies used to treat leukemia. However, such success has not been extended to the treatment of solid tumors, and the cause is being actively explored.
Multiple factors may be the cause of the successful treatment of solid tumors by CAR-T. First, even without considering the specific antigen loss or heterogeneity of the tumor, CAR-T cells must be able to successfully reach the location of the solid tumor under the premise of possible T cell chemokines and chemokine mismatches of cancer sources. And to successfully stimulate the stromal cells of the solid tumor to stimulate tumor antigen-specific cytotoxic killing. Of course, even if you successfully reach the tumor location and infiltrate it, T cells still need to overcome the challenges:
1. A tumor microenvironment characterized by oxidative stress, nutrient deficiency, acidic pH, and hypoxia.
2. Tumor-derived immunosuppressive soluble factors and the presence of cytokines.
3. Immunosuppressive immune cells, such as regulatory T cells (Tregs), bone marrow derived inhibitory cells (MDSC), tumor associated macrophages (TAM) or tumor associated neutrophils (TAN).
4. Intrinsic negative regulatory mechanisms of T cells (such as up-regulation of expression of inhibitory receptors on the cytoplasm or cell surface) and overexpression of inhibitory molecules.
5. Finally, CAR-T cells themselves can be a big problem due to their immunogenicity and toxicity.
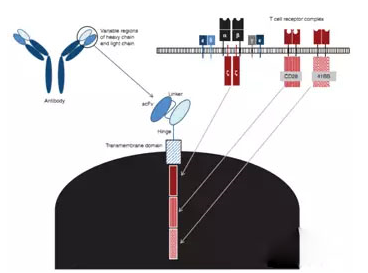
Figure 1: The "component" of CAR-T: a specific targeting antibody monoclonal (scFV) obtained from a monoclonal antibody is fused to the intramembrane domain of CD3zeta via a transmembrane domain, which is a generation of CAR-T structure. Thereafter, additional intracellular cell signaling domains have also been added, such as CD28 and 41BB, which are also referred to as 2nd and 3rd generation CARs, respectively.
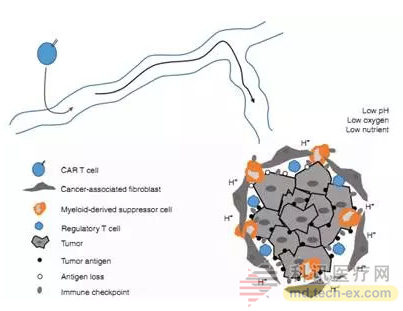
Figure 2: Immunosuppressive tumor microenvironment. This figure depicts, in a simplified cartoon form, the barriers that CAR-T cells encounter when entering a solid tumor, which inactivate CAR-T cells. All of these factors have the potential to neutralize the anti-tumor effects of CAR-T.
The Future: Understanding the Difficulties of CAR-T Therapy in Solid Tumors
It has important significance for the construction of CAR and the design of clinical programs.
There is data suggesting that lymphocyte removal may increase the potency of CAR-T. In addition, new signal domains, such as ICOS, 41BB, OX40 or CD27, are added to enhance CAR-T activation and persistence.
Source: Bio Valley
Inner Mongolia Xuanda Food Co., Ltd. , https://www.xuandagroup.com